Demand for injectable anti-obesity pharmacotherapy has reshaped many clinic schedules. Patients arrive with screenshots, brand requests, and strong expectations. Your team also carries new operational burdens. These include intake standardization, documentation, education, adverse-event follow-up, and sourcing controls.
For most practices, weight loss injections become a care pathway, not a single prescription. The operational details matter. Small gaps in training or verification can drive callbacks, missed doses, and dissatisfaction. Clear protocols help clinicians stay focused on clinical decision-making.
MedWholesaleSupplies works with licensed clinics and healthcare professionals only.
Key Takeaways
- Standardize intake: capture indications, comorbidities, prior attempts, and contraindication screens.
- Set expectations: explain variability, titration phases, and lifestyle pairing.
- Plan operations: align procurement, storage, documentation, and inventory controls.
- Use labels: confirm indications, warnings, and administration specifics per product.
Clinical Context: What Injectable Anti-Obesity Therapy Is (And Is Not)
Most prescription injectables used for chronic weight management work through incretin pathways. Incretins are gut-derived hormones that influence insulin secretion, satiety, and gastric emptying. In plain language, they can help patients feel full sooner and reduce appetite. That is often paired with improvements in cardiometabolic risk factors, depending on the patient and product.
It helps to separate medication-based weight management from cosmetic fat reduction. Patients sometimes blend the two because both are “injections.” Aesthetic fat-dissolving products are intended for localized contouring, not whole-body weight management. If your clinic fields those questions, keep a clear boundary between metabolic care and aesthetics. For background on the aesthetic side, see Fat Dissolving Injections.
Why it matters: Misaligned expectations create avoidable complaints and follow-up workload.
Where GLP-1 and dual-agonist therapies fit
Within injectables, you will hear “GLP-1 receptor agonist” (glucagon-like peptide-1 therapy) and “dual agonist” (two incretin targets). Clinics often manage requests for specific brands based on social media or peer anecdotes. Some patients also use consumer phrases like “ozempic for weight loss,” even when they do not understand indication differences. A practical response is to anchor every discussion to (1) labeled use, (2) patient safety screening, and (3) a shared plan for follow-up.
If your team wants a refresher on how GLP-1 therapy is positioned in obesity care, review Wegovy And GLP-1 Therapy. Keep the conversation clinical and documentation-forward. Patient-facing narratives tend to over-simplify expected trajectories and understate tolerability issues.
weight loss injections: What Clinics Should Standardize
Standardization protects patients and reduces rework. It also helps when multiple prescribers share coverage for the same patient panel. Start by defining what your clinic means by “eligible for medication-based weight management,” and what information must be collected before a decision is made. Policies vary by jurisdiction, payer, and clinic scope. Still, the workflow building blocks are consistent.
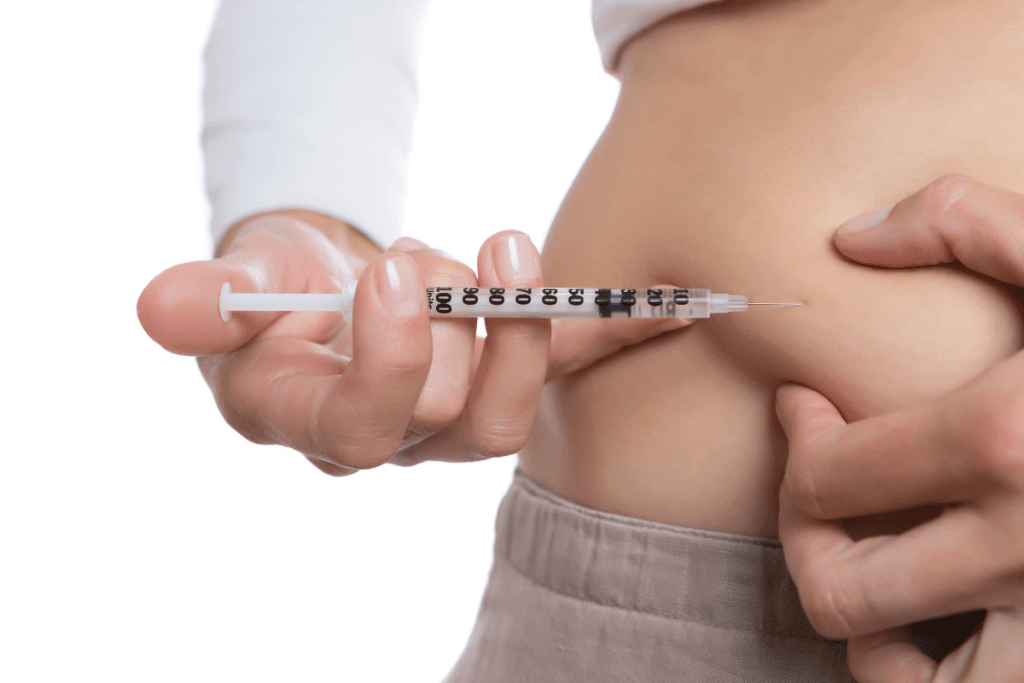
Patients frequently ask about self-administration and “weight loss injections in stomach.” Most products are designed for subcutaneous injection, often allowing abdomen, thigh, or upper arm sites per labeling. Your role is not to coach technique in an ad hoc way. Instead, create a repeatable training moment, supported by manufacturer instructions for use. Document that education occurred, and note the patient’s demonstrated understanding.
At-home administration: reduce preventable callbacks
Some searches reflect a desire for “what is the best injection for weight loss at home.” In practice, “best” usually means simplest device use, predictable access, and a follow-up cadence the clinic can support. Consider a short, standardized teaching script for nursing staff. Include injection-site rotation, missed-dose escalation pathways (refer back to the official label), and what symptoms should trigger a same-day message versus emergency care. When you do this well, you reduce medication errors and after-hours workload without drifting into individualized medical advice.
Comparing Options: What to Consider Beyond Brand Requests
Patients often arrive asking for comparisons like “mounjaro vs ozempic” or “mounjaro vs ozempic weight loss.” Clinic teams should treat these as signals to clarify goals, comorbidities, and willingness to tolerate gastrointestinal effects. Your documentation should also reflect the decision logic used, especially when you are aligning with payer policies or internal formulary approaches.
One operational advantage is to maintain a simple internal comparison framework for weight loss injections. Keep it focused on indication alignment, contraindications, device logistics, follow-up needs, and patient education burden. If you want condition-specific reading to support staff education, see Ozempic For Weight Loss and Mounjaro Weight Loss Insights.
Products may differ in labeled indications, titration schedules, and device instructions. Clinics should avoid informal “equivalency” language. That includes translating doses between products or implying interchangeable outcomes. When a patient references a “zepbound weight loss chart” or “zepbound average weight loss per month,” treat it as an opportunity to explain trial populations and variability, not as a promise. Remind staff to cite official labeling and documented clinical rationale.
How to compare: four decision factors to document
- Labeled indication: confirm the intended use matches the label.
- Contraindications: screen for key exclusions and family history flags.
- Tolerability plan: outline follow-up timing and symptom reporting pathways.
- Device handling: confirm storage constraints and patient ability to self-inject.
For clinics that stock limited on-hand units, use category hubs to keep options organized. You can browse Weight Loss Products as a high-level inventory view, without turning the care conversation into a product pitch.
Safety, Tolerability, and Monitoring Touchpoints
Most problems clinics manage are not rare events. They are predictable tolerability issues, expectation gaps, and inconsistent follow-up. GI effects are common across incretin-based therapies. They can include nausea, vomiting, diarrhea, constipation, or abdominal discomfort. The right response is a consistent triage approach aligned to labeling, with clear documentation and escalation criteria.
Patients also ask consumer-style questions like “what is the best injection for weight loss side effects.” Your staff should avoid ranking products based on anecdotes. Instead, describe that adverse-effect profiles can overlap while individual tolerability varies. Reinforce that the prescriber will consider medical history, other medications, and label warnings. If a patient asks “what is the strongest weight loss prescription pill,” the same principle applies. There is no universal “strongest” choice that ignores safety, contraindications, and adherence.
Common tolerability issues that drive clinic messages
Build templates for common contacts. For example, create a structured note for GI intolerance that captures onset timing, hydration status, ability to tolerate oral intake, and any red-flag symptoms. Add a separate pathway for suspected hypersensitivity reactions. Consider a third template for mental health changes, since patients may report mood shifts during major weight change. Do not overlook medication access lapses as a clinical risk; missed doses can trigger confusion and re-education needs. When patients present appearance concerns sometimes labeled “ozempic face,” keep the discussion neutral and evidence-based, and consider referring out if needed. Staff education can be supported by Ozempic Face Explained.
Also be clear about what your clinic does not manage. Cosmetic body contouring sits outside obesity pharmacotherapy workflows. If your practice offers both, use separate consent and documentation tracks. For broader market context, the Beauty Trends hub can help staff understand what patients are seeing online.
Cost, Coverage, and Supply Planning (Clinic Perspective)
Patients will ask about affordability, but clinics should focus on operational predictability. The drivers of weight loss injections cost are usually coverage rules, benefit design, prior authorization processes, and dispensing channel. Even when you do not handle billing, you still carry the downstream work. That includes paperwork completion, chart notes that support medical necessity, and repeated education when access changes.
Set internal expectations about turnaround times and patient communications. Avoid promising timelines. Track common denial reasons so clinicians can document more precisely on the front end. If you maintain a patient handout, keep it descriptive and label-aligned. Avoid telling patients how to “shop” for medication. That crosses into consumer guidance and can create compliance risk.
Products are brand-name items sourced through screened distribution partners.
Inventory planning should match your care model. If you administer in-office, you need clear chain-of-custody documentation and storage monitoring. If patients self-administer, your operational emphasis shifts to education, refill timing, and follow-up touchpoints. In both cases, establish a single source of truth for staff: a short internal guide that links to the manufacturer instructions and your clinic’s documentation policy.
Clinic Operations Snapshot: Verification, Documentation, and Handling
Medication-based obesity care fails operationally before it fails clinically. The most common breakdowns are missing baseline data, inconsistent follow-up scheduling, and unclear patient messaging about side effects and escalation. A simple, repeatable workflow reduces risk across all three.
Quick tip: Use one intake template across all prescribers and all locations.
Workflow (high level): from intake to follow-up
- Verify: confirm patient identity, clinical history, and contraindication screening fields.
- Document: record indication rationale, baseline metrics, and education provided.
- Procure: align sourcing to clinic policy and regulatory requirements.
- Receive: log product identifiers and inspect packaging on arrival.
- Store: follow labeled storage conditions and internal access controls.
- Dispense/admin: record lot details per your documentation standards.
- Record: schedule follow-up and capture outcomes and tolerability contacts.
For teams that need reference points on alternative injectables, some practices also keep older agents available for specific scenarios based on clinician judgment and labeling. Staff education resources include Saxenda Overview. Keep any product education aligned to the approved label and your local regulations.
Supplier verification may include licensing documentation before fulfillment.
If you source through a wholesale channel, confirm how the supplier verifies licensure, what documentation is required, and how product authenticity is supported. Many clinics also prefer stable administrative processes, such as consistent invoices and traceable receiving logs. If your operations are US-based, clarify expectations around US distribution only once in your SOPs, then keep execution consistent.
Where appropriate, you can reference specific product listings as internal staff shortcuts. Use these as identifiers, not as patient-facing marketing. Examples include Wegovy FlexTouch, Ozempic, and Mounjaro KwikPen.
For ongoing staff development, point new hires to your curated reading list. The Weight Loss Articles hub is a practical place to start.
Authoritative Sources
- FDA-approved labeling can be checked in Drugs@FDA.
- Obesity epidemiology and public health context: CDC Obesity.
- Clinical overview of overweight and obesity: NIDDK Weight Management.
Further reading works best when it supports your workflow. Choose one internal guideline for intake, one for follow-up, and one for adverse-event triage. Then train the whole team on the same documents. Consistency reduces callbacks and protects clinician time.
This content is for informational purposes only and is not a substitute for professional medical advice.