Knee osteoarthritis (OA) drives high visit volume and recurring pain complaints. Viscosupplementation (hyaluronic acid “gel” injections) is one option some practices use when conservative care is not enough. Euflexxa injections are one branded hyaluronic acid product used for intra-articular knee treatment, and they raise predictable clinic questions about procedure flow, expected timing, safety monitoring, and coverage documentation.
This briefing is written for licensed healthcare teams. It focuses on operational readiness, not prescribing decisions. Use it to align clinicians, billing, and procurement on what to verify, document, and monitor.
Key Takeaways
- Clarify patient selection criteria within your practice protocols and payer rules.
- Expect questions on onset, duration, and what “success” means in OA.
- Euflexxa injections workflow depends on clean technique, lot tracking, and consistent aftercare instructions.
- Plan for coverage documentation, including imaging and prior treatment history when required.
- Use conservative language on reviews, comparisons, and legal claims; rely on primary sources.
Why it matters: Small process gaps can create denials, callbacks, and inconsistent patient expectations.
Where Euflexxa injections Fit in Knee OA Care
Viscosupplementation knee osteoarthritis care sits between “basic” conservative measures and higher-intensity interventions. It is generally discussed for symptomatic knee OA when pain and function remain problematic despite non-procedural approaches. The clinical rationale is mechanical and biochemical: hyaluronic acid is a normal component of synovial fluid, and intra-articular supplementation may improve lubrication and shock absorption in a degraded joint environment. How much benefit a person feels can vary widely.
In day-to-day clinic language, teams may call these gel injections or rooster comb injections. “Rooster comb” is a legacy term that reflects older sourcing methods, not a single product type. Some hyaluronic acid products are avian-derived, while others are produced via non-avian processes. For patient communication, it helps to keep the explanation simple: a viscosupplement is not a painkiller injected into the bloodstream, and it is not meant to rebuild cartilage. It is a local, intra-articular therapy intended to address symptoms.
Quick Definitions
Viscosupplementation: intra-articular hyaluronic acid used for knee OA symptoms. Intra-articular: delivered into the joint space. Synovitis (joint lining inflammation): can contribute to swelling and pain. Contraindication: a situation where a treatment should not be used.
Teams also routinely ask, “is euflexxa a steroid?” It is not considered a corticosteroid injection. That distinction matters operationally, because counseling, consent language, and patient expectations often differ between hyaluronic acid products and steroid injections. When you design scripts for staff, include both terms so patients do not confuse them.
For more background on the broader category, your staff may find it useful to review the clinic-friendly overview in Types Of Gel Injections Options and the terminology explainer in Understanding Rooster Comb Injections.
Trust cue: Distribution is limited to licensed clinics and healthcare professionals.
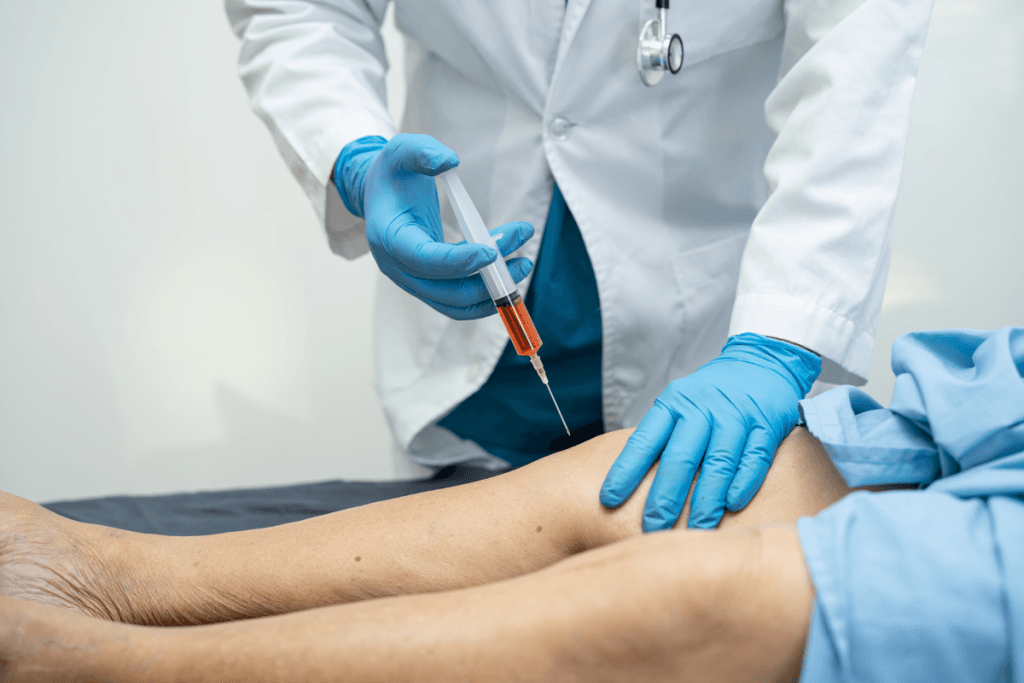
Procedure Basics and Post-Visit Aftercare
An euflexxa injection procedure in a busy practice succeeds when steps are standardized. That includes room setup, aseptic technique, timeouts, and documentation fields that are complete every time. Many clinics build a template that captures laterality, site prep, consent, lot number, expiration date, and immediate tolerance. Standardization reduces chart variance and makes audits easier.
Staff often ask, “is euflexxa injection painful?” Patient experience varies. The injection itself can be uncomfortable, and anxiety can amplify perceived pain. From a workflow perspective, the key is consistent pre-briefing: describe what the visit involves, likely sensations, and what symptoms should prompt a follow-up call. Overpromising comfort increases dissatisfaction even when the procedure is technically routine.
Aftercare Notes That Reduce Callbacks
Euflexxa injection aftercare is mostly about setting expectations and giving clear boundaries. Practices commonly provide written instructions that address activity modification for a short period, signs of a typical post-injection flare, and when to contact the office. Keep language plain and avoid implying guaranteed relief. If your clinic tracks post-procedure messages, align nurses and front desk on consistent responses and escalation triggers.
Document any immediate swelling, warmth, or vasovagal symptoms. For medicolegal clarity, also chart that the patient received written aftercare instructions and understood return precautions. If your EMR supports it, store a standardized handout in the chart for easy retrieval.
Quick tip: Add a “lot/expiry” smart field to your procedure note template.
For clinics that also manage alternative viscosupplement options, it may help to browse the orthopedic injectables hub at Orthopedic Injectables to keep your internal crosswalk of products, documentation needs, and scheduling patterns consistent.
Safety Profile: Side Effects, Warnings, and Contraindications
Most operational questions cluster around euflexxa side effects and how to triage post-injection calls. Intra-articular hyaluronic acid products can cause localized reactions such as transient pain, swelling, warmth, or effusion (fluid in the joint). Some patients describe stiffness or a flare that settles over days. While many reactions are mild, clinics should have a clear protocol for documenting, advising, and scheduling follow-up when symptoms persist or escalate.
When teams ask, “what are the problems with euflexxa injections,” they often mean two things: local inflammatory reactions and lack of meaningful benefit. For risk management, also consider procedural complications that apply to any intra-articular injection, including infection risk. You should align your consent language, sterile technique, and patient instructions with your local standards and the product labeling.
Long-Term Effects and Common Misconceptions
Patients sometimes ask about euflexxa long term side effects or systemic effects such as weight change. Hyaluronic acid injections are intended to act locally, and weight gain is not typically framed as an expected direct pharmacologic effect of intra-articular HA. Still, any new or concerning symptom report deserves clinical documentation and appropriate follow-up. Avoid dismissive language, especially when symptoms overlap with OA progression, reduced mobility, or concurrent therapies.
Euflexxa contraindications and Euflexxa warnings and precautions are label-driven topics. Clinics should avoid “memory-based” counseling and instead keep a quick reference workflow: confirm allergies and relevant history, screen for local skin infection at the injection site, and follow any product-specific precautions. If your clinic stocks multiple HA brands, ensure staff do not mix contraindication language across products.
Trust cue: Products are sourced through vetted distribution partners for authenticity.
Effect Expectations: Onset, Duration, and “Success Rate” Questions
In practice, patients and referring providers want a simple answer to “how long does it take for euflexxa to work.” The most accurate operational stance is that onset can be variable and depends on disease severity, baseline function, and patient-specific factors. Some individuals report improvement after a short interval, while others notice no change. It helps to frame timelines in terms of follow-up checkpoints rather than promises.
Similarly, “how long does euflexxa last” is better handled as a range-based expectation and a plan for reassessment. Duration of symptom relief can vary, and some patients may request repeat treatment based on prior experience and payer rules. Your scheduling team should coordinate with billing early, because repeat courses often trigger documentation checks.
The question “what is the success rate of euflexxa injections” can be hard to answer cleanly, even for clinicians. “Success” may refer to pain score reduction, functional improvement, reduced analgesic use, or delayed escalation to other interventions. Set a practice definition up front. For example, you might track a consistent patient-reported outcome measure, then use that to guide shared decision-making at follow-up visits.
When staff capture patient feedback, remind them that euflexxa injection reviews online often reflect individual experiences, not controlled comparisons. Reviews can still be useful as a signal of common concerns, like post-injection flares or frustration with slow onset. Use them to improve your scripts, not to forecast outcomes.
If It Doesn’t Help: Next-Step Planning and Alternatives
Every clinic needs a calm, consistent answer to “what next if euflexxa doesn t work.” Operationally, that starts with confirming the basics: Was the diagnosis consistent with knee OA? Was the injection visit documented correctly? Did the patient complete the planned series per the prescriber’s plan? Were there competing pain generators, such as referred pain from hip or spine? You are not changing treatment here; you are making sure the record supports the clinician’s next conversation.
Alternatives may include other viscosupplement formulations, steroid injections, physical therapy adjustments, bracing, or referral pathways. The right option varies by patient and clinician judgment, but your clinic can still standardize how you compare products and how you document prior therapies for payers.
How to Compare Hyaluronic Acid Options
If your team is asked to summarize Euflexxa vs Synvisc or Euflexxa vs Orthovisc, keep the comparison non-promotional. Focus on decision factors that affect workflow and payer interaction rather than implying superiority. Useful comparison points include labeling indications, known allergy considerations (for example, avian-derived vs non-avian sources as a general category), whether a product is typically used in a single-visit approach or a multi-visit approach, and the clinic’s ability to schedule follow-ups reliably. Always verify specifics in the current labeling and payer policy.
- Visit cadence: single vs series scheduling
- Coverage rules: prior auth and intervals
- Documentation load: imaging and prior care
- Patient factors: allergies and preferences
- Clinic capacity: room time and staffing
For deeper internal education, you can route staff to focused comparisons like Euflexxa Vs Synvisc, Euflexxa Vs Orthovisc, and Comparing Synvisc And Synvisc One. If clinicians ask about other HA options, these overviews can support neutral discussions: Hyalgan Vs Euflexxa and Supartz Vs Euflexxa.
Some practices also maintain a small set of product references for ordering consistency. When appropriate for internal cataloging, see Euflexxa Prefilled Syringes and Orthovisc as examples of how items may be listed in a procurement system.
Finally, clinics occasionally field questions about an euflexxa lawsuit. Avoid speculation and avoid counseling patients based on social media summaries. If a patient raises concerns, document the question, direct them to the official labeling and safety communications, and escalate internally to the prescribing clinician for a clinical discussion.
Clinic Operations: Coverage, Documentation, and Sourcing Controls
Coverage questions come up early, especially “does medicare cover euflexxa injections.” The practical answer is that Medicare coverage often depends on indication alignment, medical necessity documentation, and local policy details. Policies can vary by jurisdiction and by Medicare Administrative Contractor, and many commercial plans have their own rules. Build a payer matrix that lists what your clinic must capture before scheduling, such as radiographic evidence, prior therapies attempted, and symptom duration, when required.
Coverage and Prior Authorization Considerations
Billing teams can reduce rework by aligning intake, charting, and scheduling. Consider a pre-procedure checklist that confirms the diagnosis code mapping used by your clinicians, the required supporting documentation, and whether prior authorization is needed. If the payer requires a step-therapy narrative, use templated language that is factual and consistent. Avoid copying forward outdated text, especially if your clinic shifts between viscosupplement brands.
Procurement also has a role. Verify product identity, track lot numbers, and store per labeling. If you use a supplier that focuses on the professional channel, clarify how authentication and documentation are handled and what paperwork is available for your clinic records.
- Verify licensure: confirm ordering authority
- Document indication: align diagnosis and notes
- Check payer rules: prior auth and intervals
- Record product info: lot and expiration
- Store correctly: follow labeled conditions
- Administer and chart: standardized template
- Report events: adverse reaction process
Trust cue: Brand-name medical products with documentation support clinic recordkeeping needs.
Common mistakes that increase denials or callbacks include incomplete laterality documentation, missing imaging references when required, and inconsistent aftercare instructions across staff. Another frequent issue is unclear tracking of previous HA courses, which complicates repeat requests. Tighten these points in your templates and training refreshers.
- Missing lot number: harder to reconcile inventory
- Unclear laterality: billing edits and delays
- No outcome baseline: weak follow-up assessment
- Mixed scripts: inconsistent expectation setting
- Policy drift: outdated payer requirements used
For broader context on how HA injections compare across the class, see Comparing Hyalgan And Other HA and, if your clinicians discuss cross-brand expectations, Orthovisc Vs Synvisc Comparison.
Further reading: Align your internal SOPs with current labeling, payer guidance, and your clinic’s documentation standards. Revisit scripts periodically, especially after staff turnover or EMR template changes.
Authoritative Sources
- AAOS Knee Osteoarthritis Clinical Practice Guideline
- American College of Rheumatology OA Guidance
- CMS Medicare Coverage Database
This content is for informational purposes only and is not a substitute for professional medical advice.