Many practices evaluate Perfectha filler when reviewing hyaluronic acid (HA) dermal filler options. The decision is rarely just clinical preference. Procurement teams also need clear documentation, traceability, and consistent staff training. Your protocols should address product selection, patient communication, and escalation pathways for adverse events.
This guide summarizes what to confirm before adding a new HA gel line. It also highlights common operational friction points, including labeling review, storage handling, and post-procedure follow-up materials. Use it to align clinicians, practice management, and inventory control.
MedWholesaleSupplies supplies licensed clinics and credentialed healthcare teams.
Key Takeaways
- Confirm regulatory status from primary sources, not marketing materials.
- Match gel characteristics to indication and injection plane per IFU.
- Standardize documentation: lot, expiration, consent, and aftercare.
- Plan for complications with defined escalation and referral pathways.
- Use supplier verification steps to support product authenticity.
Perfectha filler in Practice: What Clinics Should Know
Perfectha is generally described as a family of HA dermal fillers. In practice, clinics consider it within a broader menu that can include other HA gels and alternative filler classes. Your early work is definitional: what the product is, what it is not, and which patient-facing claims you will avoid. Keeping that boundary tight protects both outcomes and compliance.
For operational planning, treat any new filler line like a small system change. You are adding new packaging, new IFU language, and new patient education materials. You may also add new ordering units and a revised inventory par level. A brief rollout plan reduces variation between injectors and sites, especially in multi-provider settings.
Where it fits in an HA filler menu
Most clinics organize HA fillers by expected tissue behavior and typical injection plane. You may hear teams describe gels as softer or more supportive, or discuss “lift” versus “spread.” Those are shortcuts for rheology (how a gel flows and holds shape). The safest way to operationalize those concepts is to translate them into a selection framework tied to approved labeling and injector training. For a broader review of HA in aesthetics, see Hyaluronic Acid In Aesthetics.
It also helps to define “success” in clinic terms. That often includes fewer unexpected reactions, predictable follow-up volume, and clean documentation. Before-and-after photography can be part of that system, but it should be standardized. Specify lighting, angles, and storage permissions in your consent workflow.
Formulation Basics and Product Differentiation
Most HA dermal fillers use a modified or cross-linked HA gel to increase persistence in tissue. In plain language, HA is a water-binding sugar polymer found in the body. Cross-linking changes how quickly the gel breaks down and how it behaves under pressure. Many products also include lidocaine for local anesthetic effect, which changes counseling and contraindication screening.
When clinicians ask “what is Perfectha filler,” they are usually asking about composition and portfolio structure. Confirm the ingredient list from the package insert or instructions for use (IFU). Document any local anesthetic component, and align it with your allergy screening process. If your team needs a refresher on how filler categories are commonly discussed, Types Of Dermal Fillers provides a useful overview.
Understanding Derm, Deep, and Subskin naming
Product family names often imply intended depth or typical use. Still, naming is not a substitute for labeling. If your clinicians compare Perfectha Derm vs Deep or Perfectha Subskin vs Deep, steer the discussion toward what can be verified: indicated areas, recommended injection planes, needle or cannula guidance, and any contraindications in the IFU. Build a one-page internal reference that summarizes those points and links to the official documents.
On the inventory side, keep SKUs distinct and easy to scan. For example, if you stock both Perfectha Derm Lidocaine and Perfectha Deep Lidocaine, use a receiving checklist that includes lot and expiration capture at the point of intake. That reduces charting gaps later, especially when multiple syringes are used across sites.
Clinic teams also ask about “review” signals, such as a Perfectha Subskin review. Use a hierarchy of evidence. Prioritize IFU, regulator communications, and peer-reviewed literature. Treat testimonials and non-clinical reviews as low-confidence inputs. If you still use them, use them only to generate questions to validate elsewhere.
Safety, Contraindications, and Managing Expectations
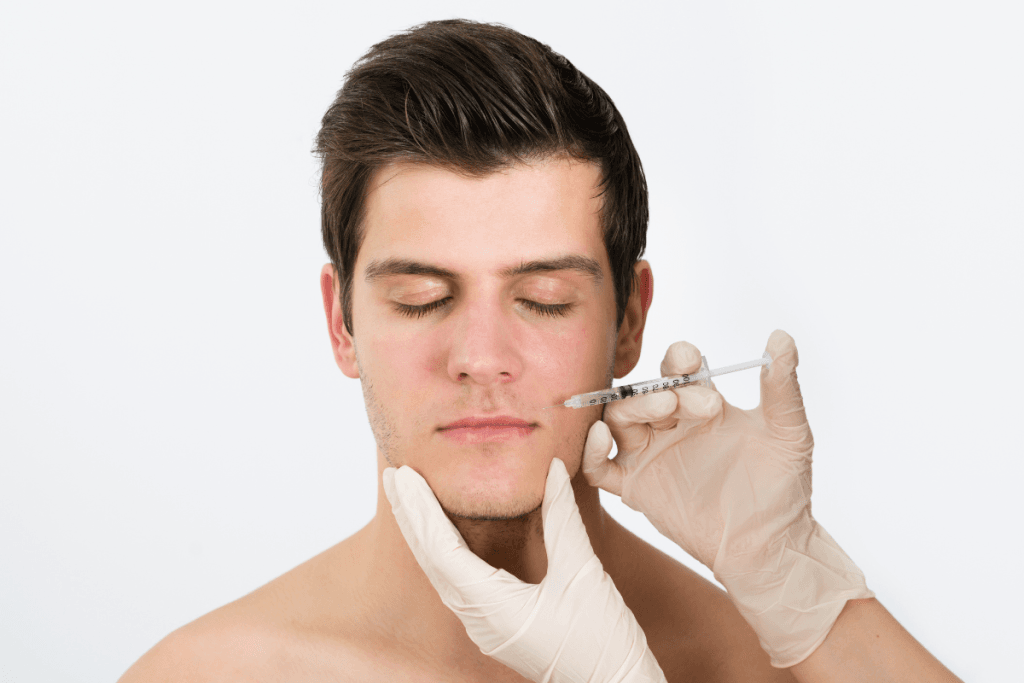
Every injectable filler program needs a shared safety language. Short-term reactions can include injection-site swelling, bruising, tenderness, and erythema (redness). Those are common across HA gels and depend on technique, tissue planes, and patient factors. Your staff should also be prepared to recognize less common complications such as delayed inflammatory reactions, nodules, infection, or vascular compromise.
Screening and consent should be consistent across providers. Focus on known allergies, prior filler history, and any conditions called out in the IFU as contraindications or precautions. Avoid “one-size-fits-all” scripts. Instead, use templated language that clinicians can personalize while remaining compliant.
Why it matters: A defined escalation pathway reduces delays when unexpected reactions occur.
Regulatory status: FDA, CE, and labeling
Clinics frequently encounter the question “Perfectha filler FDA approved.” Do not assume status from secondary sources. Confirm the product’s regulatory position using primary references and the specific product labeling for your jurisdiction. FDA status in the U.S. can differ by product, indication, and formulation, and products marketed elsewhere may carry different documentation. A CE mark indicates conformity assessment for the European market, but it is not the same as FDA approval.
Operationally, separate marketing statements from compliance facts. Keep PDFs of IFUs and any supplier-provided documentation in a controlled folder. Update it when lot formats or packaging changes. If your team needs a baseline reference on U.S. oversight and general risks, a neutral starting point is FDA information on dermal fillers and safety.
Perfectha filler safety discussions should also include training alignment. If you allow multiple injector backgrounds, define minimum competencies and documentation. Include anatomy refreshers for higher-risk zones, and require periodic review of adverse event workflows. For protocol-oriented reinforcement, see Safety-First Protocols.
Finally, manage expectations with language that is accurate and conservative. Patients may ask how long results last, or request guarantees. Keep your counseling consistent: duration varies, and outcomes depend on product selection, technique, and biology. Avoid committing to timelines in writing.
Products are sourced through vetted distributors to support brand authenticity.
Procurement, Verification, and Documentation Checklist
Adding a filler line is also a sourcing decision. Your procurement process should support authenticity, traceability, and predictable restocking. Build a supplier review that covers licensure requirements, product provenance, and the documentation you will receive with each shipment. If you maintain a preferred vendor list, define the criteria and re-check cadence.
When teams discuss Perfectha filler ingredients or “made in” details, treat those as verification items. Confirm manufacturer identity and country-of-origin statements from packaging and official documents. If a detail is missing or unclear, pause intake until you can validate it. This protects both patient safety and regulatory compliance.
Clinic documentation checklist (inventory to chart)
- License verification for purchasing account and receiving staff.
- Product name, lot, and expiration captured at receiving.
- IFU version stored in a controlled internal folder.
- Storage requirements logged and periodically audited.
- Consent templates include realistic risk language.
- Charting captures site, technique notes, and product identifiers.
- Adverse event log ties back to lot numbers.
- Photo documentation policy and retention permissions defined.
Use category hubs to keep options organized for staff. For example, your team can browse Hyaluronic Acid Fillers to compare formats and labeling needs. Keep this browsing separate from the clinical selection step. Your clinical decision-making should remain rooted in IFUs and training, not inventory convenience.
When you build a comparator set, include like-for-like product types. Many clinics cross-reference HA fillers such as Restylane 1 mL when standardizing charting fields and aftercare handouts. If you want more context for staff education, Restylane Dermal Filler Guide can support internal onboarding.
Post-Procedure Aftercare and Follow-Up Planning
Aftercare is where clinic operations become visible to patients. It is also where many avoidable calls arise. Standardize your written instructions and align them with your injectors’ actual practice. Use clear language for expected reactions like mild swelling or bruising, and state what requires prompt contact with the clinic. Avoid over-detailing medical management steps in public-facing materials.
Document “normal” and “not normal” in a way that can be audited. That includes the specific contact pathway, after-hours escalation, and how the clinic records patient-reported concerns. If your team needs a structured template, Post-Treatment Care Essentials is a helpful internal reference point.
Quick tip: Keep one version-controlled aftercare handout for each filler category.
Perfectha filler aftercare planning should also consider patient expectation management. Many patients reference social media “before and after” images. Set a policy for photo review and discussion that emphasizes variability and the limits of comparisons. If your clinic treats higher-risk areas such as under-eyes (tear trough) or lips, ensure your follow-up workflow is especially clear. Those areas can generate more swelling and more anxiety-driven callbacks.
Comparing HA Fillers Without Overpromising Outcomes
Comparisons often arise during formulary discussions: Perfectha filler vs Juvederm, or Perfectha filler vs Restylane. Keep those conversations anchored in decision factors you can document. Avoid blanket statements about superiority, duration, or “best” outcomes. Instead, build a comparison grid for internal use that links each claim to an IFU, training module, or regulator communication.
When patients ask “how long does Perfectha filler last,” clinicians may answer in ranges based on experience. For clinic documentation, however, it helps to use conservative language: longevity varies, and repeat treatment timing is individualized. Make sure your intake team uses the same language, so scheduling staff do not inadvertently promise timelines.
How to compare products for your clinic
- Labeling scope: approved areas and technique guidance.
- Formulation notes: lidocaine, HA type, handling feel.
- Risk profile: common reactions and rare complications language.
- Operations: SKU count, receiving steps, and traceability workflow.
Education links can support alignment across roles. If staff want a neutral overview of how another brand is discussed clinically, Juvéderm Treatments Overview can be used for internal training. Use it to inform questions, not to replace product-specific labeling review.
Inventory focuses on authentic, brand-name medical products for professional use.
Authoritative Sources
Use primary sources for your compliance file. That usually means the IFU, regulator communications, and documented supplier provenance. Secondary summaries can help with education, but they should not be your final reference for claims, indications, or risk language.
When policies vary by jurisdiction, default to the most conservative approach. Confirm which products are authorized where you practice, and store the relevant documents with your inventory SOPs. This is especially important when teams discuss FDA status or CE documentation.
This content is for informational purposes only and is not a substitute for professional medical advice.