Subdermal contraceptive implants can streamline contraception services when your team uses clear protocols. nexplanon implant insertion is often the operational center of that service. It combines patient counseling, a minor office procedure, documentation, and follow-up readiness. When any part is inconsistent, you see more callbacks, unclear expectations, and avoidable rework.
This guide reviews what clinics commonly standardize: candidate screening, consent language, onset timing, expected bleeding changes, and common “is this normal?” questions. It also covers removal and replacement planning, basic documentation for coding and traceability, and how to compare implants with IUDs and injections in a clinic setting.
MedWholesaleSupplies supplies inventory for licensed healthcare professionals only.
Key Takeaways
- Standardize counseling: Align timing, backup contraception, and bleeding expectations.
- Plan the full lifecycle: Schedule follow-up pathways for concerns and removal access.
- Document for traceability: Record identifiers, laterality, site, and patient counseling elements.
- Train for consistency: Use manufacturer training and internal competency checks.
nexplanon implant insertion: Clinic-Ready Overview
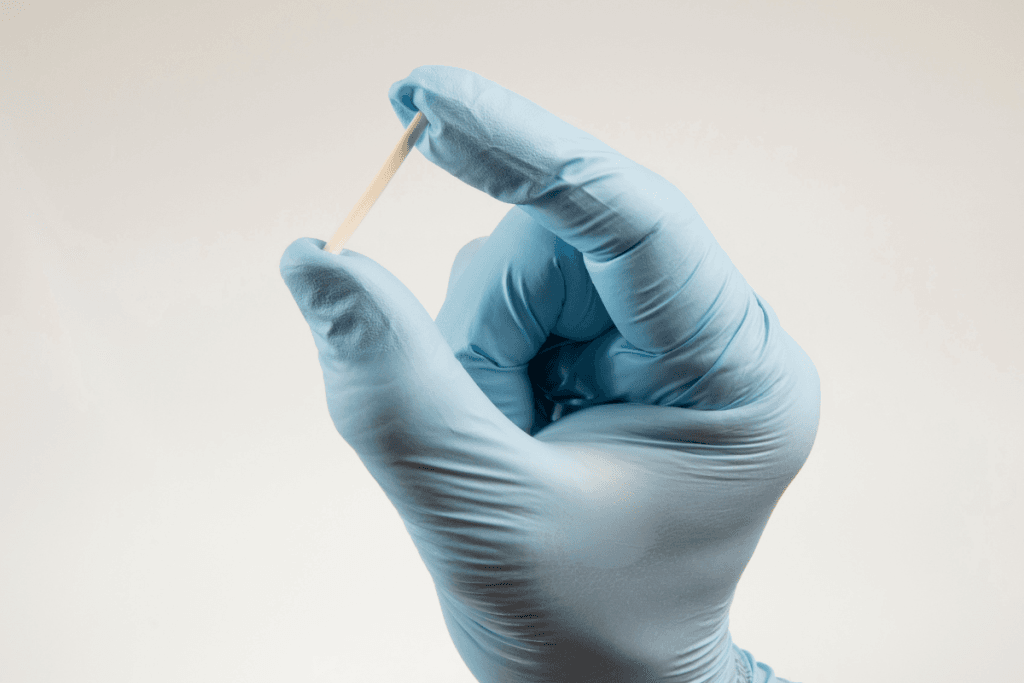
Nexplanon is a single-rod, progestin-based contraceptive implant placed subdermally in the upper arm. For many practices, it functions like a “procedure visit” rather than a typical prescription refill. That difference matters for staffing, rooming, supplies, and charting. A reliable workflow lowers variability across clinicians and reduces after-hours questions.
Clinic teams usually separate the service into three parts: (1) pre-visit screening and consent, (2) the procedure and immediate aftercare, and (3) a defined pathway for later concerns. Even when the clinical act is brief, the surrounding steps drive most of the operational load. Build templates that make those steps hard to miss.
Nexplanon Implant Listing can help procurement teams align item selection with internal formularies and lot tracking.
Technique updates and location guidance
Many teams field questions about the “new insertion site” guidance that circulated in recent years. In practice, your priority is to follow the current manufacturer training and labeling for placement location and technique. Updated location guidance is generally intended to reduce risk near neurovascular structures. That operational takeaway is simple: keep competency current, do periodic peer observation, and document site and laterality clearly. If you use training videos, make sure they match the current instructions, not legacy content saved on a shared drive.
Quick tip: Store a single “current training link” in your procedure note template.
Screening, Consent, and Setting Expectations
Pre-visit screening prevents most day-of delays. Your intake should confirm the patient’s goals, current method, timing of last unprotected intercourse, and any symptoms that warrant pregnancy assessment. Clinics often use a short, standardized script for counseling because patients may arrive with mixed information from social media and forums.
At the consent step, the operational goal is consistent, plain-language communication. Use both clinical terms and patient-friendly phrasing. For example, counsel on irregular bleeding and amenorrhea (no periods) without predicting a specific pattern. Document that bleeding changes are common and can include spotting, longer bleeding, or no bleeding.
When clinicians ask for a clean “start” protocol, remind teams that timing depends on cycle timing and prior contraception. nexplanon implant insertion often triggers questions about whether backup contraception is needed. The safest approach is to reference the official labeling for timing rules and your practice protocol, rather than ad hoc counseling.
Explaining onset and the “7-day” message
Patients frequently ask why it takes 7 days for contraception to “work.” This is usually a counseling shorthand for “backup is recommended for a brief period” depending on timing of insertion and the prior method. Operationally, you want staff to avoid absolute statements. Train them to say, “The need for backup depends on when it’s placed and what you used before,” then point to your written handout. If your clinic provides emergency contraception counseling when appropriate, ensure the message is consistent with your broader contraception policy and local regulations.
Why it matters: Timing confusion drives repeat calls and avoidable urgent visits.
Expected Effects and How to Triage Safety Signals
Most post-placement questions cluster into two categories: bleeding changes and arm symptoms. Bleeding changes can persist or evolve over time, so patients may report “new” symptoms months later. For clinic operations, the key is to define what is expected, what is bothersome but non-urgent, and what warrants timely evaluation.
Teams should be prepared for questions framed as “nexplanon side effects after 1 year” or “nexplanon side effects after 2 years.” Patients often interpret timing as a sign of failure. In reality, symptom timing does not automatically indicate reduced effect. Your triage protocol should focus on severity, associated symptoms, and pregnancy risk, not the calendar alone. When patients report systemic symptoms, use a structured review and consider other causes, rather than attributing everything to the implant.
Arm complaints also vary. Early tenderness and ecchymosis (bruising) are common after minor procedures. Later localized pain raises different considerations. When someone reports “sharp pain after insertion,” staff should ask about distribution (localized versus radiating), sensory changes like paresthesia (tingling), redness, drainage, or fever. For “why does my nexplanon hurt months later,” consider assessment for local scar sensitivity, positional irritation, or other pathology, and document exam findings carefully.
MedWholesaleSupplies sources brand-name products through vetted distribution partners.
Pitfalls clinics can avoid
- Overpromising bleeding patterns: Avoid “your period will stop” guarantees.
- Missing pregnancy triage: Have a script for symptoms and testing pathways.
- Vague arm symptom notes: Record location, neuro symptoms, and palpability.
- Ignoring patient language: Translate “wearing off” into objective questions.
Aftercare, Healing, and Common Patient Questions
Post-procedure instructions work best when they are written, consistent, and easy to find in the portal. Patients search for practical questions like “when can I shower” and “can I lay on my arm,” and they will fill in gaps with whatever they find online. To reduce confusion, align nursing scripts with what clinicians document in the plan.
Most clinics cover basic wound care and activity guidance without making it sound like a strict rulebook. You can use ranges and conditional language. For example, many practices advise keeping the dressing on for a defined period, minimizing friction, and avoiding soaking the site early on, but specifics should match your protocol and labeling. Use plain-language terms such as “keep the area clean and dry” alongside clinical terms like “monitor for erythema (redness) or drainage.”
During nexplanon implant insertion counseling, set expectations for the healing timeline in general terms. Patients often expect the site to feel “normal” immediately. Let them know mild tenderness can persist, and bruising can change color before fading. Also explain what should prompt a call, such as increasing swelling, spreading redness, fever, or significant arm numbness.
After-visit handout checklist
- Bandage plan: What to keep, replace, remove.
- Hygiene guidance: Showering and soaking instructions per protocol.
- Expected symptoms: Bruising, mild soreness, spotting possibilities.
- Red flags: Fever, drainage, worsening pain, numbness.
- Contact pathway: Daytime phone and after-hours instructions.
Removal, Replacement, and Documentation Standards
Removal planning is part of quality contraception care, not an afterthought. Patients may request removal for bleeding changes, mood concerns, or pregnancy planning. Others come in because of online stories, including “nexplanon removal reddit” threads. A clinic-ready approach is to define access: how quickly you can schedule removal visits, what documentation you need before the appointment, and who performs complex removals when the rod is difficult to palpate.
From an operations standpoint, nexplanon implant insertion and removal should share a documentation backbone. Capture the procedure date, laterality, insertion site description, and identifiers used for traceability. Teams also ask about nexplanon removal icd-10 selection. Coding depends on the encounter context and payer guidance, so many practices build a billing cheat sheet that is reviewed periodically rather than relying on memory.
If you offer same-visit replacement, set clear scheduling rules. Patients may ask, “Can you get pregnant after getting Nexplanon replaced?” Avoid absolutes. Use your protocol to address timing, pregnancy assessment when indicated, and whether backup contraception is recommended.
For procedure supplies and instruments, many clinics maintain a dedicated pick list and restock par levels. A browseable hub like Gynecology Tools can support standardization across rooms.
Clinic workflow snapshot (high-level)
- Verify: Confirm patient identity and consent elements.
- Document: Template note, laterality, site description, counseling points.
- Receive: Log item identifiers and expiration dates per policy.
- Store: Follow manufacturer labeling and internal inventory controls.
- Administer: Procedure, site check, and immediate instructions.
- Record: Update problem list/contraception history and billing details.
Some organizations prefer reliable US logistics for predictable restocking across multiple sites.
Comparing Implant Services With IUDs and Injections
Clinics typically compare the implant with hormonal IUDs, copper IUDs, and injectable contraception. Each choice changes visit cadence, procedure time, and follow-up patterns. Keep the comparison practical: staffing needs, typical counseling load, and what “failure concerns” look like in real workflows.
In many practices, nexplanon implant insertion competes operationally with IUD insertions because both require procedure rooms, trained staff, and standardized aftercare. Injectable methods, by contrast, often shift the burden to repeat visits and reminder systems. If your clinic provides multiple methods, align patient education materials so staff do not inadvertently frame one method as universally “better.”
| Service type | Typical clinic drivers | Common follow-up contacts |
|---|---|---|
| Implant | Procedure slot, trained inserter, device traceability | Bleeding changes, arm tenderness, “wearing off” concerns |
| Hormonal IUD | Pelvic procedure setup, pregnancy screening, strings counseling | Cramping, bleeding pattern questions, string checks |
| Copper IUD | Pelvic procedure setup, bleeding expectations counseling | Heavier menses concerns, cramping, expulsion worries |
| Injection | Repeat visit system, standing orders/policies, inventory cycles | Scheduling adherence, bleeding changes, longer-term tolerability |
When discussing alternatives, link your counseling to the services you actually deliver. For teams offering injections, these internal primers can help align terminology: Hormonal Injection Overview and Depo-Provera Overview. For longer-term management conversations, Depo-Provera Long-Term Use provides a structured discussion frame.
For method availability in your inventory, you may cross-reference items your clinic already stocks, such as Mirena IUD Listing, Copper IUD Listing, or Depo-Provera Listing.
How to interpret online reviews and forum posts
Patients often arrive with screenshots of “nexplanon reviews” or forum threads about removal experiences. Your staff can acknowledge the experience without validating every claim. A useful script is: “People’s bleeding patterns and side effects vary, so we focus on your symptoms and your goals.” Then translate emotional language into clinical triage questions: onset, severity, associated symptoms, and functional impact. This approach reduces defensiveness and improves documentation quality. It also helps you decide whether a visit needs counseling time, an exam, pregnancy testing, or referral for a complex removal.
If your clinic also counsels on emergency contraception, keep comparisons neutral and policy-based. This overview may help staff handle “backup” questions consistently: Emergency Contraceptive Comparisons.
Authoritative Sources
Use primary sources to keep counseling and protocols aligned with current evidence and labeling. This is especially important for timing rules, contraindications, and any updates to technique or post-procedure guidance. When you update templates, document the source and date so staff can cite it consistently.
For clinic training, consider building a short reference list inside your EHR order set. Keep it limited to documents you can maintain. If you support multiple clinicians, standardizing around two or three sources reduces variability in patient messaging and lowers follow-up friction.
- FDA labeling database for product prescribing information
- CDC contraception guidance and U.S. recommendations
- ACOG clinical guidance and practice resources
Further reading works best when it supports your workflow: pick one counseling handout, one triage script, and one documentation template, then keep them current.
This content is for informational purposes only and is not a substitute for professional medical advice.