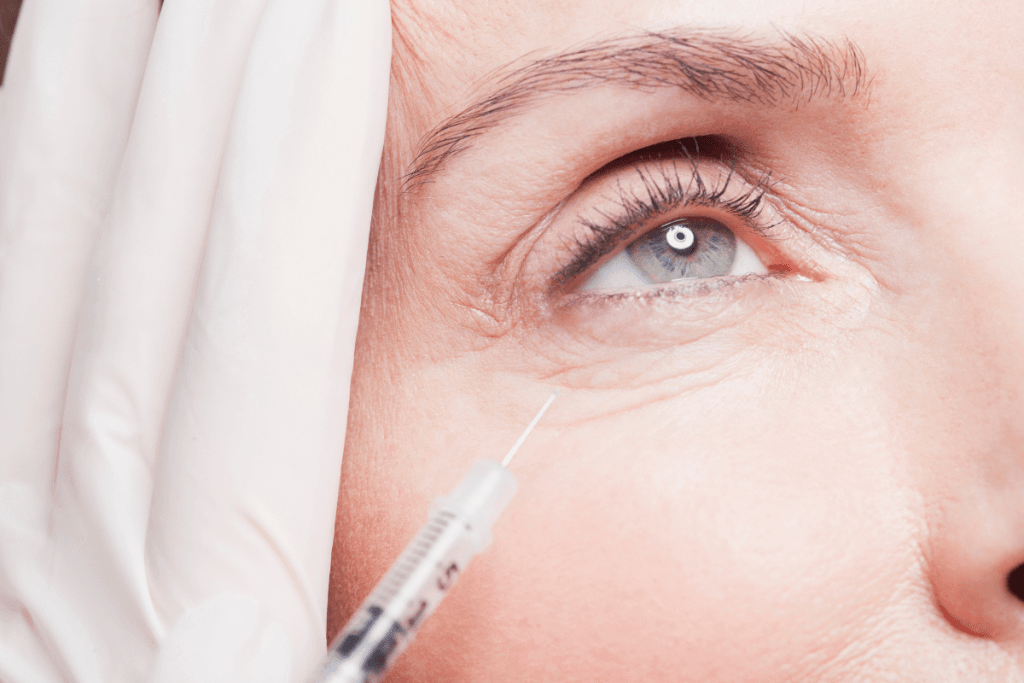
Periorbital treatments sit at the intersection of aesthetics and function. Small changes around the lids and brow can shift expression, comfort, and patient satisfaction. When you evaluate botox for eyes in your clinic, the risk profile is different than midface work. Anatomy is tighter, muscle balance matters, and minor asymmetries can look dramatic on camera.
Clinics also face practical questions. How do you set “before and after” standards? What do you document for medical indications like blepharospasm (involuntary eyelid closure)? And how do you discuss longevity and cost without overpromising results? Supply access is typically limited to verified licensed healthcare accounts.
Key Takeaways
- Periorbital goals depend on muscle balance, not a single injection point.
- Standardized photos and symptom tracking reduce disputes about outcomes.
- Under-eye treatment has higher visibility and higher downside risk.
- Medical coverage requires documentation that supports medical necessity.
- Procurement workflows should track lots, storage, and authorized users.
Where Periorbital Neuromodulators Fit in Aesthetic Plans
Most eye-area requests relate to dynamic rhytids (wrinkles) created by repetitive muscle activity. Common cosmetic targets include lateral canthal lines (“crow’s feet”), glabellar complex activity that can pull the brow down, and certain patterns of under-eye creasing that appear when smiling. Patients may also ask for “hooded eyes botox before and after” images, expecting a brow or lid change. In practice, those changes depend on baseline brow position, eyelid skin redundancy, and how strongly the frontalis and brow depressors recruit.
Periorbital neuromodulation can also show up in medically oriented workflows, such as management of blepharospasm or hemifacial spasm (intermittent unilateral facial contractions). These cases bring different documentation needs, follow-up cadence, and payer scrutiny. The same molecule class may be used, but the clinic process often looks more like a procedure pathway than a cash-pay aesthetic visit.
Why it matters: Around the eyes, subtle imbalance can read as “complication” even when medically minor.
| Presentation | What patients mean | Common clinic discussion points |
|---|---|---|
| Lateral canthal lines | Crow’s feet at rest or smiling | Dynamic vs static lines; realistic smoothing expectations |
| Under-eye creasing on smile | “Wrinkles when smiling” | Skin texture vs muscle; higher risk of lid heaviness |
| “Jelly roll” | Infraorbital roll with smile | Conservative planning; monitor lid support and dry eye risk |
| “Open the eyes” | Less heaviness, more lid show | Brow position drivers; avoid promising lid lift |
| Eyelid twitch or spasm | Annoying contractions | Rule-outs; procedure documentation; payer requirements |
From an education standpoint, many clinics find it helpful to show patients several reference categories. “Botox for eyes before and after” images can be framed by expression type (smile, squint, neutral) and by priority (smoothing, symmetry, comfort). Some practices also standardize how they label common requests like “jelly roll botox before and after” to prevent mismatch between patient vocabulary and clinical assessment.
For deeper background on common target zones, you can cross-reference your internal protocols with a site-based overview such as Botox Injection Sites. Keep your discussion high-level in patient materials. Reserve technique details for clinician training and the product labeling.
Botox for eyes: Mapping Goals to Muscles
In periocular work, patients often describe a single “problem,” but the driver is usually a pattern. Lateral orbicularis oculi activity can create crow’s feet. Corrugator and procerus activity can influence brow position and the appearance of “11 lines.” Overactivity in depressor muscles can contribute to a tired look, which is why “botox to open eyes before and after” searches are common. The practical takeaway is that you are managing a system, not a line.
For clinic teams, a simple framework helps. Start with the primary complaint, then map it to the muscle group, then identify compensations. That approach prevents over-treating the under-eye when the visible issue is actually brow depression or midface skin quality. It also supports consistent charting when patients compare “full face botox before and after” expectations to a limited periorbital plan.
Periorbital assessment that supports safe planning
Document what you see before you propose a plan. Note baseline brow height, eyelid show, asymmetry, and any history of ptosis (lid droop). Ask about dry eye symptoms and contact lens tolerance, since ocular surface comfort can influence perceived outcomes. Assess whether lines are dynamic, static, or largely textural. Many “under eye botox before and after” requests are actually about skin crepe, pigment, or tear trough contour, which may not respond well to neuromodulation alone.
Also clarify what the patient calls “under-eye wrinkles when smiling.” Some patients point to infraorbital orbicularis recruitment (“jelly roll”), while others mean lateral canthal lines that extend under the eye. This distinction matters for risk management and for how you set expectations around function, especially blinking strength and lid support.
From a procurement and compliance angle, practices often keep a short list of vetted neuromodulator options for clinician preference and formulary consistency. If you maintain brand-specific protocols, link your inventory notes to the exact product received (for example, Botox, Dysport, Azzalure, or Letybo 50U English). Products are brand-name items obtained through screened distributors.
Expected Course, Longevity, and “Before/After” Evidence
Clinics get asked “how long does botox last” in nearly every periorbital consult. A practical way to answer is to speak in ranges and variability drivers. Duration can depend on treated area, baseline muscle strength, individual metabolism, and how consistently a patient returns for maintenance. Many practices plan a reassessment window rather than a fixed expiration date, especially when the patient is new to neuromodulation or has complex asymmetry.
“Before and after” management is often where operational friction arises. Patients may arrive with screenshots labeled “botox before and after 11 lines” or “botox for under eye wrinkles when smiling before and after,” then assume identical outcomes. Your best defense is consistent imaging and documentation, not longer consult scripts.
Photo and symptom documentation that holds up over time
Standardize lighting, camera distance, and expression prompts. Capture neutral, full smile, and tight squint views. Add a short set of clinician-noted descriptors in the chart, such as “dynamic lateral canthal lines,” “infraorbital roll present on smile,” or “baseline right brow lower.” When a patient asks about botox for eyes cost or longevity, you can tie your response back to the documented baseline and planned scope, instead of debating a social media comparison.
For therapeutic use cases, add a symptom-focused baseline. Frequency of spasms, functional impact, and prior treatments matter for continuity of care and payer review. For additional context on duration expectations and how clinics discuss them, see Duration Of Botox Effects. Keep your clinic’s statements conservative and aligned with the prescribing information.
Managing Risk: Selection, Counseling, and “Under-Eye Gone Wrong” Narratives
Periorbital adverse outcomes are disproportionately visible. Even when medically mild, they can create strong dissatisfaction and reputational risk. Patients searching “under eye botox gone wrong” typically describe lid heaviness, asymmetry, altered smile dynamics, or a sensation of dryness. Some of these outcomes relate to diffusion into nearby muscles. Others reflect a mismatch between what neuromodulation can do and what the patient actually wanted (often texture, laxity, or volume support).
Risk mitigation starts before consent forms. Use plain-language explanations alongside clinical terms. Explain that orbicularis oculi contributes to blinking and tear pumping, and that altering it may change comfort in some patients. Clarify that static under-eye crepe may need a different modality, such as skin-directed treatments or, in selected cases, volume correction. This is also where “under eye wrinkles botox or filler” becomes a useful comparison point, as long as you avoid pushing a single solution.
- Baseline lid laxity present: flag higher heaviness risk
- Dry eye history: consider comfort implications and expectations
- High camera sensitivity: reinforce photo standardization and angles
- Prior periocular surgery: document and consider specialist input
- Strong asymmetry: define what “improvement” means in writing
Patients may also ask about twitching. “Does eye twitching after botox go away” can refer to benign eyelid myokymia (small muscle quiver) or to a return of underlying spasm when effects wear off. It can also be unrelated to treatment. If the visit includes medical spasm management, keep documentation clear about the indication and functional impairment. For safety counseling language and general side-effect framing, you can align staff education with Botox Side Effects.
Technique questions also surface in medical contexts. People search “where do they inject botox for eye twitching” and “hemifacial spasm botox injection technique,” but clinics should avoid sharing injection mapping outside clinician education. In general terms, medical spasm treatment often targets affected facial muscles, commonly including periocular muscles, with dosing and placement guided by labeling, training, and patient response. For these cases, ensure that an experienced injector manages the plan and that follow-up is documented as part of a procedure workflow.
Cost Conversations and Coverage Basics for Clinics
Periorbital pricing questions are persistent, and they often arrive bundled with internet terms like “under eye botox cost,” “botox cost calculator,” or “how much does a 50 unit vial of botox cost.” In a clinic setting, it helps to separate three things: acquisition costs (what your practice pays), professional fees (time, expertise, overhead), and variability driven by treatment scope. Because acquisition costs can vary by supplier relationships and ordering structure, many practices avoid quoting vial-based figures in consults.
Instead, consider a standardized internal estimator that accounts for the planned regions and follow-up touchpoints. Your staff can describe how your clinic builds a treatment plan, what is included in the visit, and how follow-up is handled. That approach answers the real question—predictability—without turning a clinical service into a commodity comparison.
Coverage questions require even more structure. “How much does botox cost with insurance” and “does insurance cover botox for eye twitching” depend on indication, documentation, and payer policy. Cosmetic periocular treatments are typically not covered. For medical indications like blepharospasm, payers may require a documented diagnosis, symptom severity, and prior therapies, plus prior authorization. Build templates for these records, and keep them consistent across providers. For comparative education on product differences that may affect clinic operations, see Botox Vs Dysport Analysis.
When patients ask about trends, it can help to point clinicians to a curated hub rather than scattered posts. A category view like Beauty Trends can help staff understand common patient language and expectations, while keeping your own counseling grounded and conservative.
Clinic Operations Checklist: Product Controls and Records
Periorbital work runs smoother when your operations match your clinical standards. That includes consistent receiving, inventory controls, and lot-level documentation. MedWholesaleSupplies is structured for licensed healthcare professionals and clinics, with brand-name products supplied via vetted distribution channels. Your internal policies should still assume audits can happen, and that charts may be reviewed for medical necessity when you treat functional indications.
Quick tip: Use one template for periocular consent, then add indication-specific addenda.
Workflow snapshot for periocular neuromodulators
- Verify: confirm authorized purchasers and clinician users
- Document: capture baseline photos and symptom notes
- Receive: record lot, expiration, and condition on arrival
- Store: follow label storage requirements and access controls
- Administer: chart indication, regions, and follow-up plan
- Record: link outcomes and any complaints to the lot number
For clinics that manage multiple toxins, keep product selection and staff education aligned. A simple internal reference can link to your formulary list, plus a browseable category like Botox Category for procurement teams who need to confirm SKU naming and packaging formats. This reduces errors when new staff members handle ordering or receiving.
Finally, ensure your patient education stays distinct from your procurement pathway. Your internal inventory notes can reference specific products, but patient-facing materials should stay focused on goals, risks, and follow-up expectations. This separation helps prevent confusion when patients search brand names and assume interchangeability.
Authoritative Sources
Use primary sources for labeling, boxed warnings, and approved indications. This is especially important when patients ask about medical spasm treatment, dosing units, or off-label considerations for the under-eye area.
- FDA Drug Labels (search for onabotulinumtoxinA)
- American Academy of Ophthalmology
- American Academy of Dermatology
For further reading, keep your team aligned on language, documentation, and patient expectations. If you standardize assessment, photography, and inventory records, botox for eyes discussions become clearer and disputes become easier to resolve.
This content is for informational purposes only and is not a substitute for professional medical advice.