Patients arrive with strong expectations for neuromodulator injections, often shaped by social media. Your role is to translate that demand into a safe, documented, and consistent process. A well-structured consult reduces surprises, supports informed consent, and protects clinical workflow. Using the same core questions to ask before botox also helps your team communicate clearly across locations and providers.
In practice, most “Botox” requests are shorthand for several botulinum toxin type A options. Product selection, dilution approach, unit conventions, and follow-up norms can vary by practice. The consult is where you align patient goals with realistic outcomes and risk tolerances. It is also where you identify red flags early, before chair time is committed.
Supplies are intended for verified licensed healthcare accounts.
For first-time patients, clarity matters more than volume. A brief, repeatable script supports clinical judgment without turning the visit into a lecture. It also creates a consistent patient experience, even when you rotate injectors. Later in this guide, you will see how to group questions to ask before botox into documentation-ready categories.
Key Takeaways
- Standardize consult topics to reduce missed history details.
- Document indication, product, lot, and injection plan consistently.
- Explain units as product-specific and non-interchangeable.
- Set expectations on onset, duration, and follow-up windows.
- Build an aftercare handout aligned to your protocol.
Clarify the Product, the Goal, and the Treatment Map
Many patients use one brand name as a generic term. Start by confirming what they mean: cosmetic rhytid reduction (wrinkle-softening) versus medical indications, and which areas they want treated. In plain language, you are mapping “where the muscle moves” to “what the patient notices.” This early clarification prevents a later mismatch between the requested area and the likely effect.
It can help to show a standardized facial or anatomic diagram. Document the target areas, the patient’s primary concern (for example, “forehead lines” versus “brow heaviness”), and any asymmetry at rest and in animation. If your team needs a quick refresher on common regions, link staff to an internal primer such as Injection Sites Overview. For clinics managing multiple toxin brands, keeping a shared reference list can also reduce ordering errors; see Popular Botulinum Toxin Brands.
Units are a frequent point of confusion. A “unit” is not a universal dose like mg or mL. Potency units are product-specific, and units should not be converted across brands as if they were equivalent. Your documentation should therefore capture the product name, units used, and rationale for the plan. For procurement and formulary review, many practices maintain a hub page for what they stock, such as a Botox Category that organizes brand options for internal review.
questions to ask before botox: A Clinic-Ready Framework
A consult framework works best when it is predictable. You can use the same sequence across patient types, then adapt the depth. This keeps the visit efficient and supports consistent charting. It also makes handoffs easier when a different injector performs follow-up.
Start with goals, context, and prior exposure
Ask what outcome they want in everyday terms. Some want “no movement,” while others want “softening only.” Clarify timelines tied to events, travel, photography, or work demands. If they have had prior neuromodulator injections, document product used, perceived duration, any adverse effects, and satisfaction with the result. For patients switching products, note whether they are comparing brand names or comparing a prior injector’s technique. If your staff needs deeper reading on brand-to-brand considerations, a neutral internal explainer like Botox Vs Dysport Analysis can help standardize language.
Use documentation prompts you can chart quickly
Most missed details fall into a few repeatable categories: health history, medications, expectations, and aftercare constraints. A template makes it easier to capture the same data in every visit. The table below is designed to fit a standard consult note without implying a specific medical decision.
| Consult topic | What to capture | Why it matters |
|---|---|---|
| Goal and priority | Primary concern, acceptable trade-offs | Aligns plan to patient-defined success |
| Prior injections | Product, timing, response, problems | Helps anticipate expectations and tolerance |
| Medical history | Neurologic, swallowing/breathing issues, infections | Supports risk screening and documentation |
| Medication list | Prescription, OTC, supplements, recent antibiotics | Identifies potential bleeding or interaction concerns |
| Aftercare fit | Workouts, facials, travel, follow-up access | Reduces preventable dissatisfaction |
Why it matters: Standardized notes reduce variability when multiple injectors share a patient panel.
Finish by reviewing what is known, what is uncertain, and what will be reassessed at follow-up. Patients often accept “may” and “can” language when you explain that individual response varies. Confirm that they understand the plan is a clinical procedure with potential risks, not a guaranteed cosmetic outcome.
Screening, Contraindications, and Medication Review
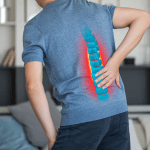
Screening should be structured and recorded in a way that is easy to audit later. Focus on conditions that could change risk, consent, or timing. That includes neuromuscular disorders, active infection at the injection site, prior hypersensitivity reactions, and any history of swallowing or breathing difficulties. When information is incomplete, document what was asked, what was answered, and what remains unknown.
Medication review is often where workflow breaks down. Patients may not consider supplements “medications,” and they may forget intermittent agents. Your intake should explicitly include OTC analgesics, anticoagulants or antiplatelets, herbal products, and recent antibiotics. Avoid giving individualized stop/start instructions in generic materials; instead, document what the patient reports and follow your clinic’s protocol for clearance when needed.
For pregnancy and lactation, many practices treat elective cosmetic injections as a defer-and-revisit topic. Document pregnancy status when relevant, and confirm the patient’s understanding of your policy. If they are breastfeeding, chart the discussion and defer to product labeling and clinician judgment. In the same visit, you can place the patient’s questions to ask before botox into the chart as part of informed consent, even if treatment is deferred.
Products are sourced through distributor partners with documented provenance.
Finally, confirm the patient’s ability to comply with follow-up and aftercare. If they are leaving town immediately, have limited ability to return, or have upcoming procedures, note those constraints. These operational details often predict dissatisfaction more than technique does.
Setting Expectations on Results, Risks, and Longevity
Expectation-setting is not a one-time disclaimer. It is a short, specific conversation that mirrors how your clinic actually follows patients. Explain typical onset in general terms: many patients notice changes within several days, and the maximal effect may take up to about two weeks. Duration varies by patient, area treated, and technique, and effects often lessen over several months. Consider routing staff to a deeper internal review like Duration Of Botox Effects to keep language consistent across providers.
Discuss adverse effects using neutral, non-alarming language. Common issues can include injection-site pain, swelling, bruising, headache, or localized weakness. Less common but clinically important risks include spread of toxin effect beyond the injection site. For teams that want a structured overview, see Botox Side Effects Overview and, for a specific symptom discussion some patients ask about, Post-Injection Headaches.
Quick tip: Use the same “common vs serious” phrasing in every consent discussion.
Practical comfort questions come up in nearly every visit. “Does it hurt?” is often about anxiety, not needle size. Describe the sensation plainly and outline what your clinic typically uses for comfort measures, without promising a pain-free experience. If bruising is a concern, avoid making medication changes via generic advice; instead, document risk factors and explain that bruising can still occur even with careful technique.
Aftercare instructions should be consistent with your practice protocol and the product labeling. Many clinics advise avoiding pressure or massage over treated areas for a period of time, and they may counsel patients to avoid certain activities immediately after treatment. Provide a written handout, document that it was given, and note any exceptions. This is also a good point to revisit questions to ask before botox that relate to scheduling, exercise routines, and follow-up access.
Clinic Workflow and Supply Chain Considerations
Operational reliability supports clinical reliability. A standardized workflow reduces missed steps in verification, storage, and lot tracking. It also makes adverse event documentation cleaner if issues arise. For clinics adding new toxin options, keep a simple formulary note on what is stocked and why. Examples of product pages used for internal reference include BOTOX, Dysport, and Xeomin.
Documentation should not end at consent. Record product name, lot number, expiration date, preparation details per your protocol, injection plan, and any immediate reactions. Confirm that your inventory process supports traceability across locations and staff. If you supply multiple brands, keep units and dilutions clearly separated in storage and in the EHR pick-list to avoid charting errors. For practices reviewing additional options, a page like Nabota 200UI can serve as a reference point for procurement discussions, without replacing label review.
Only authentic, brand-name items are supplied to professional practices.
Clinic workflow snapshot (generic)
- Verify account credentials and documentation requirements.
- Confirm product selection and internal formulary approval.
- Receive shipment and log lot/expiration on arrival.
- Store and handle per current labeling and SOPs.
- Document administration details in the medical record.
- Schedule and record follow-up assessment when used.
Supplier selection is part of risk management. Use partners that support licensed-clinic purchasing and documentation, and keep records of invoices and provenance. If you operate across multiple sites, decide where inventory is held and how transfers are logged. When clinics rely on US distribution, reconcile receiving logs with the clinical schedule to avoid last-minute substitutions.
From a patient-experience perspective, consistency is the point. When your intake, consent language, and aftercare handouts match, your team spends less time correcting misunderstandings. That is the operational payoff of using the same questions to ask before botox across providers and locations.
Authoritative Sources
This content is for informational purposes only and is not a substitute for professional medical advice.