Key Takeaways
Hyaluronidase for lip filler is typically used to reverse hyaluronic acid gel in selected situations. This page reviews concepts, safety points, and clinic-ready workflow elements.
- Confirm filler type: HA dissolves; many biostimulatory fillers do not.
- Plan for adverse events: allergy risk and vascular compromise require readiness.
- Standardize documentation: product, lot, assessment findings, and follow-up notes.
- Set expectations: swelling, bruising, and transient texture change can occur.
Overview
Lip filler corrections can be time-sensitive and emotionally charged. Clinics often need a clear, repeatable approach for assessment, consent, aseptic preparation, and follow-up. The goal is consistent decision-making, not speed.
In practice, hyaluronidase for lip filler is most relevant when the injected material is hyaluronic acid (HA, a gel-like sugar polymer). It may be considered for issues like overcorrection, contour irregularity, or suspected vascular occlusion (blocked blood vessel). For broader context on correction pathways, see Dermal Filler Removal Options for a structured overview. MedWholesaleSupplies operates as a credentialed, clinic-facing supplier, supporting licensed teams that need verified sourcing for brand-name injectables.
Core Concepts: Hyaluronidase for Lip Filler
What hyaluronidase does (and does not do)
Hyaluronidase is an enzyme that breaks down hyaluronic acid in tissue. In plain terms, it can “loosen” or reduce HA gel and endogenous HA in the immediate treatment area. That mechanism is why it is used to address unwanted HA filler outcomes in the lips and perioral region.
It is equally important to define limits. Hyaluronidase does not reverse non-HA fillers in a predictable way. Calcium hydroxylapatite (CaHA, a mineral-based gel) and poly-L-lactic acid (PLLA, a collagen-stimulator) behave differently, and management may involve observation or specialist referral depending on the presentation. If your team needs a refresher on filler categories, HA Vs Non-HA Fillers provides a practical comparison.
Common clinical scenarios in the lip and perioral area
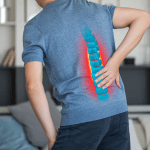
Lip anatomy increases the chance that small asymmetries become obvious. Patients may present with a palpable ridge, visible lumps, or uneven vermilion border definition. Others describe “migration” or heaviness, which may reflect product placement, edema (swelling), or changes in dynamic movement rather than true product displacement.
Clinics also see color changes such as Tyndall effect (blue-gray hue from superficial HA). In the lips, subtle superficial placement can show quickly in certain lighting. Another frequent complaint is “wrinkly lips after dissolving,” which can reflect rapid deflation, transient swelling, or pre-existing perioral rhytids becoming more visible when volume is reduced. Discuss this risk in consent language and chart it as an expectation-setting point.
Spread, diffusion, and why mapping matters
Teams often ask how far hyaluronidase spreads. There is no single distance that applies to every patient, because diffusion depends on injection plane, local tissue architecture, edema, prior filler distribution, and technique. Lips are particularly dynamic and vascular, so small placement differences can change observed effects.
A practical approach is to map findings before any intervention. Use consistent lighting, standardized photos, and a structured palpation exam. Consider marking subunits where the contour issue is most evident. This reduces “over-dissolving” driven by guesswork. For general injection risk reduction concepts, Safety First Protocols is a useful internal reference for team training.
Safety considerations and adverse event planning
Any use of hyaluronidase should be framed as a clinical procedure with meaningful risks. Hypersensitivity reactions are a central concern, ranging from localized reactions to anaphylaxis (severe allergic reaction). Review contraindications and warnings in the specific product labeling your clinic uses, and align your workflow with facility policy.
Another high-stakes scenario is suspected vascular compromise after filler placement. In that context, “emergency protocol” language is common, but protocols vary by jurisdiction and medical direction. Your clinic should define roles, escalation steps, and documentation expectations ahead of time. Injection Safety can serve as a hub for related operational content.
Note: Online searches about “lip filler dissolver side effects” often blend true adverse reactions with expected post-procedure swelling and bruising. Clinic handouts should separate expected effects from red flags.
Practical Guidance
For many practices, hyaluronidase for lip filler fits best into a standardized correction pathway. The pathway should emphasize patient assessment, informed consent, and readiness for adverse reactions. It should also define when to pause and refer, especially when the presentation is atypical.
Start by confirming what was injected and when, using available records. If the product is unknown, document that uncertainty and how it affects planning. Your team can also keep a quick reference to filler families through the Dermal Fillers category hub, which supports product-type literacy for staff.
Clinic checklist (non-prescriptive)
- Intake details: prior filler type, site(s), and reported timing.
- Focused exam: symmetry at rest and animation, palpation, mucosal inspection.
- Risk screen: allergy history and prior reactions to injectables.
- Consent points: under/over-correction risk, swelling, bruising, texture change.
- Photo protocol: consistent angles and lighting for follow-up comparison.
- Emergency readiness: clinic policy for hypersensitivity response and escalation.
Reconstitution and handling: build it into your SOP
Queries like “how to reconstitute hyaluronidase,” “how much saline to mix,” or “1500 IU dilution” are common online. However, reconstitution steps must be taken directly from the specific product monograph or manufacturer instructions for use, plus your medical director’s standing orders. Different presentations and brands can have different requirements and compatibility notes.
Operationally, clinics benefit from a short SOP that covers aseptic technique, labeling of prepared solution, beyond-use expectations per policy, and segregation from look-alike vials. If you stock multiple brands, keep packaging images in your training file. For clinics that maintain a dedicated correction inventory, Dermal Filler Removal is a useful navigation point for organizing internal purchasing lists without turning protocols into product-specific instructions.
Tip: Add a documentation line for vial lot and expiry in the procedure note.
Compare & Related Topics
Clinicians frequently get asked about “how to dissolve filler naturally at home” or “how to dissolve filler without hyaluronidase.” Those phrases reflect patient anxiety and misinformation, not safe clinical pathways. Massage, heat, or supplements should not be positioned as reliable reversal methods for injectable gels. The safer response is education, assessment, and an evidence-based plan matched to the filler type and symptoms.
Use the comparison below to support consistent internal triage. It helps staff explain why some fillers can be enzymatically reduced, while others cannot. For myth-busting language you can adapt to counseling scripts, Dermal Filler Myths is a practical companion resource.
| Topic | HA (hyaluronic acid) fillers | Non-HA fillers (biostimulatory or mineral-based) |
|---|---|---|
| Reversal concept | May be enzymatically reduced | Not reliably reversed with enzyme |
| Examples (non-exhaustive) | Many common gel fillers used for lips | CaHA, PLLA, PCL-based options |
| Common correction pathways | Assessment, targeted correction, follow-up | Observation, targeted management, referral as needed |
| Key operational need | Clear consent and adverse reaction readiness | Product identification and expectations management |
Clinic Ordering and Compliance Notes
When clinics stock hyaluronidase for lip filler, the operational goal is consistency. That includes credentialing, traceable sourcing, and controlled access within the practice. Many teams also maintain a small set of standardized supplies, such as blunt cannulas, to support predictable technique choices across providers.
For product navigation, some clinics reference the Hyaluronidase Brand Hub to keep internal ordering lists organized. Examples of listings include Hyaluronidase 1500 UI and Liporase Hyaluronidase 1500U, which clinics may evaluate based on labeling, packaging, and internal policy. If your workflow uses cannulas for selected corrections, SoftFil Micro Cannula is a relevant reference point for supply standardization.
Ordering through MedWholesaleSupplies is restricted to licensed clinics and healthcare professionals, with account verification aligned to regulated distribution. The platform’s role is B2B supply through vetted channels, which supports clinic documentation and traceability expectations during audits.
Authoritative Sources
Because hyaluronidase products vary by source material, concentration, and approved indications, use the specific label that matches your stocked product when building protocols. Avoid copying dosing tables from informal “protocol PDFs” circulating online, since they may not match your formulation, jurisdiction, or medical direction.
These references are useful starting points for clinic policy review and staff education on warnings and administration considerations for hyaluronidase for lip filler:
Recap: Focus first on filler identification, risk screening, and documentation. Use product-specific labeling and clinic policy for preparation and administration details. Maintain a clear escalation plan for suspected complications.
This content is for informational purposes only and is not a substitute for professional medical advice.
________________________________________________________________________________________
Medically Reviewed by: Ma Lalaine Cheng.,MD.,MPH