Platelet-rich plasma (PRP) has become a common adjunct in musculoskeletal care. Clinics are asked to explain it clearly, set realistic expectations, and document each step. orthopedic platelet rich plasma therapy sits at the intersection of clinical judgment, procedure technique, and operational discipline.
This briefing focuses on how PRP is typically used in orthopedics and sports medicine. It also covers preparation choices, ultrasound workflow, and safety monitoring. The goal is a practical, compliance-forward view that supports consistent clinic processes.
Key Takeaways
- Define PRP simply and consistently
- Match PRP type to tissue context
- Standardize prep and documentation
- Track outcomes with repeatable measures
orthopedic platelet rich plasma therapy: What It Is and Why It Matters
PRP is an autologous blood product. “Autologous” means it comes from the patient. Whole blood is processed to concentrate platelets in plasma. Platelets contain signaling proteins that can influence local biology. These are often described as growth factors (cell-signaling proteins). Clinics may use PRP to support a broader care plan for degenerative and overuse conditions.
PRP is not one standardized drug. It is a preparation with meaningful variability. Key variables include baseline platelet count, centrifugation approach, platelet concentration, and leukocyte (white blood cell) content. Activation method and injectate handling also differ. These choices can affect inflammatory response, post-procedure pain, and how clinicians interpret outcomes across patients.
PRP mechanism of action, in plain terms
PRP is generally discussed as a biologic “signal booster.” Platelets release mediators that can influence inflammation and tissue remodeling. In practice, PRP may be used where clinicians aim to modulate symptoms and support function, especially when mechanical loading and rehabilitation are also addressed. Evidence is mixed across conditions and protocols, so many practices treat PRP as one option within shared decision-making rather than a universal solution.
Supply partners often restrict distribution to licensed clinics and credentialed healthcare professionals.
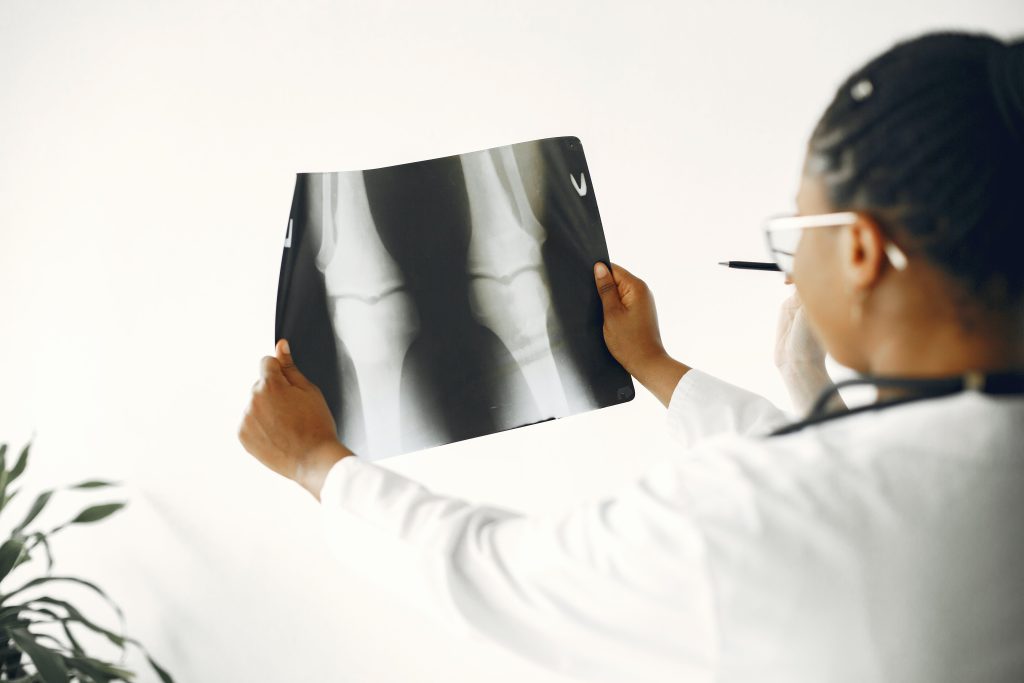
Where PRP Is Considered in Orthopedics and Sports Medicine
In musculoskeletal care, PRP is most often discussed for tendinopathy (degenerative tendon pain), selected ligament injuries, and symptomatic osteoarthritis. Common examples include PRP injections for knee osteoarthritis and platelet rich plasma for tendon injuries such as lateral epicondylitis (tennis elbow) and plantar fasciitis. Some clinicians also consider PRP for rotator cuff tears, Achilles tendinopathy, and patellar tendinopathy, typically alongside structured rehabilitation and load management.
Meniscal pathology and focal cartilage lesions are more variable areas. PRP for meniscus tears and PRP for cartilage regeneration are both active topics, but the quality of evidence and protocol consistency can differ by study design. PRP for bone healing is also discussed in certain orthopedic settings, though many practices treat this as an evolving use case rather than routine care.
When your team reviews treatment pathways, it helps to benchmark PRP against other injection families already in use. For a broad overview of options and typical clinic decision points, see Knee Pain Injection Options and Non-Surgical Joint Pain Alternatives.
Selection signals and red flags to document
Most clinics document clinical context rather than promising outcomes. That includes symptom duration, prior conservative management, imaging reports when relevant, and baseline functional limits. They also record factors that could affect PRP quality or procedural risk. Examples include bleeding disorders, platelet dysfunction, active infection, or use of medications that affect coagulation. Contraindications and precautions vary by protocol and local policy, so keep a standardized screening template and update it when your procedure committee updates protocols.
Why it matters: Consistent selection documentation reduces variability when you review outcomes later.
Preparation Choices, Protocol Variability, and Supply Readiness
PRP preparation methods and protocols are a core source of variability. Clinics typically define the centrifugation method (single- vs double-spin), anticoagulant use, target cellular profile, and handling steps from draw through injection. Even when the clinical indication is similar, protocol choices can differ by provider preference, published methods, and internal quality review. If your clinic supports multiple provider styles, consider a small set of approved “house protocols” with clear naming and documentation fields.
Operationally, treat PRP like a procedure with a defined bill of materials. That includes sterile disposables, collection tubes, labels, and a plan for chain-of-custody within the clinic. Some practices also keep adjunct items on hand for specific workflows. For example, if your team uses PRP gel formats in certain settings, you may want a designated inventory lane for related consumables such as Plasmolifting PRP Gel Tubes, based on your internal protocols and applicable regulations.
Leukocyte-rich vs leukocyte-poor PRP: operational implications
Leukocyte-rich vs leukocyte-poor PRP is a practical distinction clinics often discuss. Leukocyte content can influence the inflammatory milieu after injection. Some protocols aim to reduce leukocytes for intra-articular use, while others accept higher leukocytes for certain tendon applications. The key operational point is not “which is best,” but “which is intended.” Your documentation should capture the intended PRP type and how it was produced, so chart reviewers can interpret outcomes and adverse events in context.
Inventory is typically obtained through vetted distribution channels with traceability expectations for clinical use.
Checklist: what to standardize before first case
- Protocol naming + version control
- Staff roles per step
- Labeling and time stamps
- Centrifuge maintenance logs
- Consent + aftercare handouts
- Adverse event documentation pathway
- Outcome measures and intervals
PRP dosing and frequency are often asked about by patients and staff. Avoid embedding rigid schedules into patient-facing materials unless your medical leadership approves a condition-specific protocol. Instead, document that timing and number of injections vary by indication, clinician assessment, and response, and that the plan is individualized within your clinic’s policy.
Ultrasound Guidance, Injection Technique, and Safety Monitoring
Ultrasound-guided PRP injection is widely used to improve anatomic accuracy, especially for tendon insertions and peri-tendinous targets. Workflow matters. Your clinic should standardize probe covers, sterile gel use, skin prep, and image storage rules. Decide how images are attached to the chart, how laterality is labeled, and who verifies documentation completeness.
PRP injection side effects are usually local and self-limited, such as post-injection soreness, swelling, or a pain flare. However, PRP risks and complications can include infection, bleeding, vasovagal events, and damage from inaccurate needle placement. Document risk counseling, sterile technique steps, and post-procedure instructions. Align incident reporting with your broader injection safety program.
Quick tip: Use a single “procedure note shell” for all injectables, then add PRP-specific fields.
Pitfalls that create avoidable variability
- Unlabeled PRP preparation method
- Missing laterality and target site
- No baseline functional score recorded
- Inconsistent post-procedure restrictions
For clinics that also provide other injectables, cross-training helps reduce errors. Consider maintaining one hub for injectable workflows and supplies, such as your Orthopedic Injectables category list, with internal notes on which items support which pathway.
How to Compare PRP With Other Orthopedic Injections
When patients ask “PRP vs corticosteroid injection” or “PRP vs hyaluronic acid,” the most useful answer is often about goals, tradeoffs, and evidence certainty. orthopedic platelet rich plasma therapy is usually framed as a biologic approach, while steroids are anti-inflammatory drugs and hyaluronic acid (HA) is a viscosupplement (joint lubricant-like polymer). Many clinics present these as different tools, each with its own risk profile, expected onset pattern, and durability in published studies.
If your team wants internal consistency, define a few comparison points that are always covered: expected symptom targets, typical counseling points, common adverse effects, and what follow-up looks like. For broader reading on HA pathways and how clinics discuss gel injections, review Types Of Gel Injections and Cortisone And HA Injections.
| Approach | What it is | Common clinic considerations |
|---|---|---|
| PRP | Autologous platelet concentrate | Protocol variability; consent and outcome tracking are essential |
| Corticosteroid | Prescription anti-inflammatory injection | Short-term symptom control; document glucose and tissue considerations per policy |
| Hyaluronic acid | Viscosupplement injected into joint | Product-specific labeling; series rules vary by payer and guideline |
When HA is part of your pathway, keep product documentation tight. Even within the same class, handling, syringe formats, and labeling differ. If your clinic needs examples for reference, see items like Orthovisc and Hyalgan, and connect those to your internal ordering and charting checklists. For an HA-specific clinical comparison discussion, you can also read Comparing Hyalgan Options.
Recovery, Follow-Up, and Outcomes Tracking That Hold Up
PRP recovery and aftercare planning should be written in plain language. Patients often interpret soreness as “something went wrong,” so your materials should define expected post-procedure discomfort and what changes warrant contacting the clinic. Avoid absolute promises about when someone will feel better. Instead, document a follow-up cadence, the outcome measures you will recheck, and how rehab coordination will be handled.
PRP treatment timeline discussions are especially prone to misunderstanding. Many clinics avoid fixed time guarantees and focus on milestones. Examples include short-term safety check-ins, return-to-activity planning with physical therapy, and reassessment windows for function and pain scores. This is also where you can standardize how you discuss PRP for sports injuries, since athletes often focus on readiness, not just pain relief.
From an operations standpoint, it helps to track PRP success rates in orthopedics within your own dataset, using consistent measures and definitions. Do not market internal numbers as generalizable. Use them for quality improvement, protocol refinement, and clinician education. Products supplied are typically brand-name and authenticity-verified through supplier controls.
Clinic workflow snapshot (high-level)
- Verify patient identity and laterality
- Document screening and consent
- Prepare sterile field and ultrasound setup
- Process sample per named protocol
- Perform injection and record images
- Provide standardized aftercare instructions
- Record outcomes and any adverse events
For knee-specific pathway discussions that your staff can reference, see Orthovisc Vs Synvisc. If you use sports medicine counseling language for HA or related injectables, Hyalgan In Sports Medicine can help standardize talking points and documentation prompts.
Authoritative Sources
For evidence summaries and regulatory context, keep a short list of neutral references your team can revisit during protocol review.
- American Academy of Orthopaedic Surgeons PRP overview
- FDA consumer alert on regenerative medicine marketing
- NIAMS osteoarthritis background and care concepts
This content is for informational purposes only and is not a substitute for professional medical advice.